PRESSURE ULCER / BED SORE PRODUCT REFERENCE GUIDE
PRESSURE ULCER STATISTICS:
- More than 2.5 million people develop bedsores at a cost of more than $10 billion each year.
- Each pressure wound adds $43,180 to the cost of a hospital stay.
- More than 34,000 people die from infection and other complications due to bedsores yearly.
Pressure Ulcers are also referred to as Bed Sores. Below is our Pressure Ulcer reference guide. It should only be used as a guide to help you consider which products may be appropriate in the prevention and treatment of pressure ulcers / bed sores.
Prevention is Key:
Pressure ulcers / Bed Sores are much easier to prevent than they are to treat. Proactively addressing the factors listed below greatly improves prevention. The most important factor is reducing the pressure between the skin and the surface below. This is accomplished by using a pressure redistribution cushion, mattress, pillow or overlay, depending on your specific needs, before a pressure ulcer occurs.
Proactive Treatment:
Once a pressure ulcer occurs it can be extremely painful and the source of a potentially fatal infection. Pressure ulcers are rated in stages I - IV. In any stage, proactive treatment is the only way to prevent progression and promote healing. The stage rating of the ulcer will determine which products / therapies are appropriate to promote healing. A pressure redistribution cushion, mattress, pillow or overlay, that addresses specific needs, must be considered.
FACTORS THAT CONTRIBUTE TO PRESSURE ULCERS
Pressure Ulcers (bed sores) are an injury to the skin and underlying tissue caused by multiple factors including:
- - Interface Pressure between the skin and a surface restricts / interupts blood flow to the skin
- - Temperature
- - Moisture
- - Shearing Forces
- - Friction
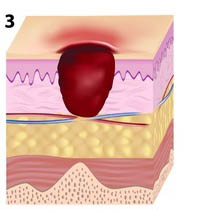
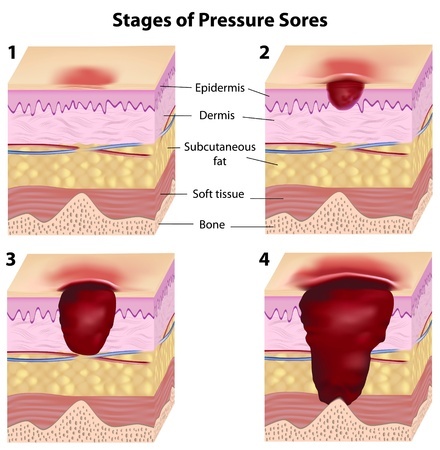
PRESSURE ULCER STAGES
Pressure Ulcers are described or rated in stages that can range from mild reddening of the skin to severe tissue damage. This includes open wounds that extend into the muscle or bone making a person susceptable to very difficult to treat and potentially fatal infection.
 STAGE I
STAGE I
The skin may be red and painful, but it has no breaks or tears. The skin appears reddened and does not lose color briefly when you press your finger on it and then remove the pressure. In a dark-skinned person, the area may appear to be a different color than the surrounding skin, but it may not look red. Skin temperature is very often warmer and can feel either firmer or softer than the area surrounding it.
What to do about a Stage I Pressure Ulcer
- Use an appropriate cushion, mattress or overlay to redistribute pressure.
- Keep the area clean and dry.
- Reduce heat build up between the skin and the support surface.
- Find and remove the cause.
- Inspect the area at least twice a day.
- Call your health care provider
- Healing Time Estimate: Three Days
- GOOD = FOAM
- BETTER = GEL OR SELF ADJUSTING AIR
- EVEN BETTER = ALTERNATING PRESSURE
- BEST = ALTERNATING PRESSURE WITH LOW AIR LOSS
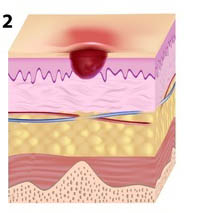 STAGE II
STAGE II
The skin is broken and wears away,or forms an ulcer, which is most often tender and painful. The sore expands into deeper layers of the skin often appearing as an abrasion, blister, or a shallow crater. Blisters are often filled with clear fluid and some skin may be necrotic (dead) and damaged beyond. ***Bruising may indicate deep tissue injury.
What to do about a Stage II Pressure Ulcer
- Use an appropriate cushion, mattress or overlay to redistribute pressure.
- Keep the area clean and dry.
- Reduce heat build up between the skin and the support surface.
- Reduce miosture build up between the skin and the support surface.
- Find and remove the cause.
- Inspect the area at least twice a day.
- Call your health care provider
- Healing Time Estimate: Three Days to Three Weeks
- GOOD = GEL OR SELF ADJUSTING AIR
- BETTER = ALTERNATING PRESSURE
- BEST = ALTERNATING PRESSURE WITH LOW AIR LOSS
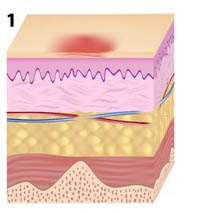
STAGE III
The ulcer extends deeper into the tissue beneath the skin, forming a crater. The sore may be so deep that fat may show in the sore. However, not muscle, tendon, or bone. In stage III pressure ulcers where there are deep tissue wounds, there may be little or no pain. Serious and potentially fatal infection of the bone (osteomyelitis) or blood (sepsis), can occur.
What to do about a Stage III Pressure Ulcer
- Use an appropriate cushion, mattress or overlay to redistribute pressure.
- Keep the area clean and dry.
- Reduce heat build up between the skin and the support surface.
- Reduce miosture build up between the skin and the support surface.
- Find and remove the cause.
- Wounds need frequent special care.
- See your health care provider.
- Healing Time Estimate: One to Four Months
- GOOD = ALTERNATING PRESSURE
- BEST = ALTERNATING PRESSURE WITH LOW AIR LOSS
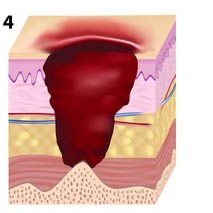 STAGE IV
STAGE IV
The pressure sore is very deep, reaching into muscle and bone and causing extensive damage. Damage to deeper tissues, tendons, and joints may occur. In stage IV pressure ulcers where there are deep tissue wounds, there may be little or no pain. Serious and potentially fatal infection of the bone (osteomyelitis) or blood (sepsis), can occur.
What to do about a Stage IV Pressure Ulcer
- Use an appropriate cushion, mattress or overlay to redistribute pressure.
- Keep the area clean and dry.
- Reduce heat build up between the skin and the support surface.
- Reduce miosture build up between the skin and the support surface.
- Find and remove the cause.
- Wounds need frequent special care.
- See your health care provider.
- Healing Time Estimate: Three Months to Two Years
- BEST = ALTERNATING PRESSURE WITH LOW AIR LOSS
- BEST* = AIR FLUIDIZED THERAPY (AFT) *For Burns and Flap Surgeries
Not all pressure ulcers fit into the categories above. Sometimes a doctor is unable to determine the stage of a pressure ulcer due to a number of possible factors. The pressure ulcer is considered "unstageable". In other cases there is no open wound however, the underlying tissue has been damaged. This is called a DTI or deep tissue injury.
SUMMARY
- Pressure ulcers are common, costly conditions.
- Pressure ulcers can be prevented
- A standard hospital mattress has an interface pressure of 100 mmHg which can result in pressure ulcers unless repositioning occurs at regular intervals.
- Interface pressure can be reduced using support surfaces (either static [non-powered] or dynamic [powered]).
- Alternating Pressure with Low air loss (LAL) and air fluidized therapy (AFT) are the major types of dynamic support surfaces for the prevention of pressure ulcers in high-risk patients.
- Moisture accumulation on the skin is an important physical factor predisposing a patient to the occurrence of pressure ulcers and tissue breakdown.
- Temperature management has a critical effect on skin health.
****The guide above should not be used to treat, diagnose or accurately determine the stage of a pressure ulcer. It should be used as a simplified reference only.
information sources:
http://www.msktc.org/sci/factsheets/skincare/Recognizing-and-Treating-Pressure-Sores,
http://www.patientcare-edu.com/imageServer.aspx?contentID=20368&contenttype=application/pdf
http://www.npuap.org/resources/educational-and-clinical-resources/npuap-pressure-ulcer-stagescategories/